CVS Health Corporation Faces Medicaid Lawsuit: Key Details and Industry Impact
CVS Health Corporation, a leader in American healthcare and pharmacy services, finds itself at the center of a significant legal dispute. Recent whistleblower allegations accuse the company of overbilling state Medicaid programs—a claim that has captured attention across the industry. This article breaks down the lawsuit, reaction from stakeholders, and the broader implications for healthcare compliance.
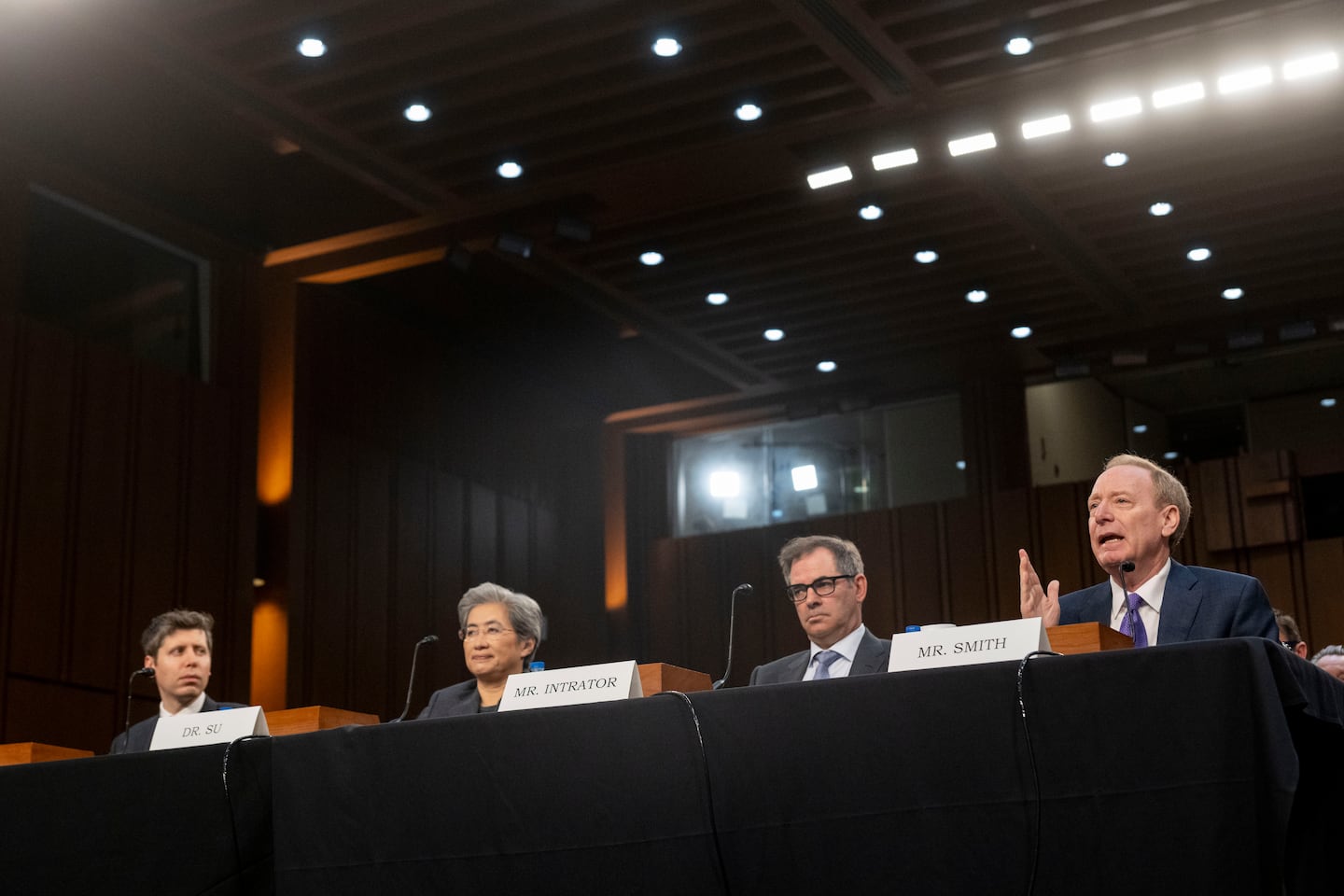
Customers visiting a CVS Health Corporation pharmacy location. CVS has been a central player in pharmacy services across the United States.
Background: Whistleblower Allegations Against CVS Health Corporation
In May 2025, a coalition of state attorneys general filed suit against CVS Health Corporation. The allegation is that its pharmacies overbilled Medicaid for prescription drugs by failing to report the lowest available prices—required under state and federal law.[^1] According to the lawsuit, CVS offered discounted drug prices to cash-paying customers via programs such as ScriptSave, while allegedly not passing those discounts on to Medicaid programs like MassHealth.
These practices have been under scrutiny since at least 2016. In its defense, CVS Health Corporation strongly denies any wrongdoing. The company states that state regulators never clarified whether third-party discount card prices should be considered the “usual and customary” rate for Medicaid.[^2]
Key Details of the Lawsuit
- Reporting Practices: Attorneys general argue that pharmacies must bill Medicaid programs the lowest price charged to any customer. This is to ensure fair pricing for taxpayers and Medicaid recipients.
- Impact on MassHealth: Massachusetts Attorney General Andrea Joy Campbell emphasized that offering lower prices to private customers without extending them to Medicaid violates state law.
- CVS’s Position: CVS insists it has always been transparent with Medicaid and disputes that its pricing was inflated. Previous similar cases have either been dismissed or decided in favor of CVS.[^1][^2]
For a comprehensive description of the ongoing legal proceedings and statements from parties involved, you can review the detailed coverage at HealthExec.
Broader Industry Implications
This legal battle shines a spotlight on pharmacy benefit management and healthcare compliance in the United States. Many pharmacies, not just CVS Health Corporation, face questions about their billing practices and transparency with Medicaid programs. Ensuring fair drug pricing is critical for both public trust and health system sustainability.
For additional insight into the regulatory dimensions and local government response, read the Boston Globe’s analysis on how these allegations have stirred debate in Massachusetts and beyond.
What Comes Next for CVS Health Corporation?
The lawsuit is still in its early stages, and federal courts have yet to rule on the core claims and compliance questions. CVS Health Corporation, meanwhile, maintains its innocence and commitment to transparency in pharmacy operations. Industry observers and stakeholders watch closely, knowing that this case could influence future pharmacy regulations and Medicaid reimbursement procedures.
Stay tuned to local outlets like Franklin Observer for updates on community perspectives and responses.
Conclusion
As CVS Health Corporation navigates these legal challenges, the case underscores the importance of compliance, transparency, and fair pricing in American healthcare. For consumers, taxpayers, and industry leaders alike, the outcome will likely shape pharmacy policies in the years ahead.
[^1]: CVS Health sued by coalition of states alleging Medicaid fraud by pharmacies
[^2]: AG alleges CVS didn’t share discounts with MassHealth members - The Boston Globe